Essential characteristic of the study cohort
Finally, 7110 pregnant women were included in this study. All patients were divided into five groups according to their HPV infection status, Group I (n = 216), Group II (n = 655), Group III (n = 414), Group IV (n = 135), and control Group (n = 5690).
The primary clinical information for all patients is shown in Table 1. There was no statistical difference in the clinical basis information of the five groups in this study. The mean age of the study cohort was 31.1 ± 4.3 years. Of all pregnant women, 2753 (38.7%) had once gravity, 2160 (30.4%) twice gravity, and 2195 (30.9%) three times gravity. Also, 4271 (60.1%) 0–1 parity, and 2839 (39.9%) twice parity. Of the 7110 newborns, 3716 (52.3%) were males and 3394 (47.7%) were females. And then, the mean gestational age at delivery was 38.6 ± 2.1 weeks. The mean birth weight was 3237.9 ± 516.5 g, and the mean baby height was 49.3 ± 2.6 cm.
Continuous variables are presented as mean ± SD (range), ANOVA was used for comparison, and categorical variables as n (%), Chi-square test was used for comparison.
GA, gestational age; HPV, Human papillomavirus; Control group means without HPV infection; Group I means low risk HPV infection; Group II means infection with nine-valent HPV vaccine covered high-risk HPV subtypes; Group III means infection with non-nine-valent HPV vaccine covered high-risk HPV subtypes; Group IV means co-infection with nine-valent HPV vaccine covered high-risk HPV subtypes and non-nine-valent HPV vaccine covered high-risk HPV subtypes.
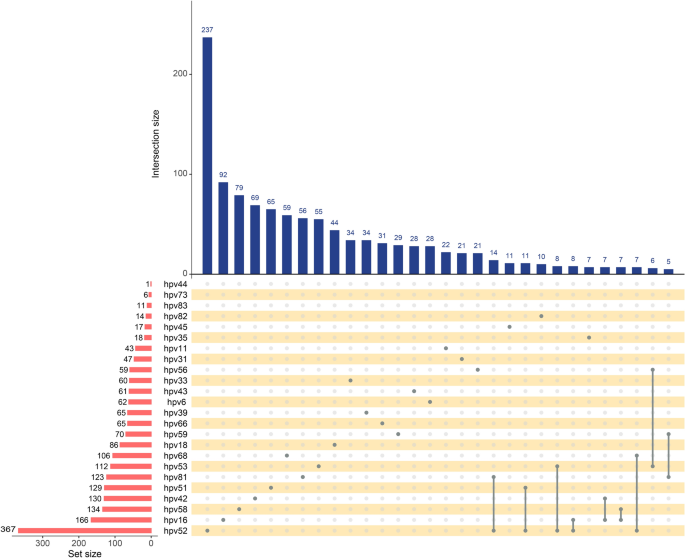
Distribution of infection rates of HPV subtypes
The infection of different HPV subtypes in all participants is shown in Fig. 1. Our results suggested that most pregnant women are HPV negative, followed by 9.2% of pregnant women with low-risk HPV infection (group I ), group II (5.8%), group III (3.0%), and group IV (1.9%). We then analyzed the specific HPV subtypes and found that HPV 52, 16, 58, 42 and 51 were the five most common infection types. The above HPV subtypes were high-risk HPV infections except HPV 42. Also, most of these HPV infections are isolated infections. Co-infection with HPV 52 and HPV 81, HPV 52 and HPV 51 is the most common type of multiple infection.
Distribution of all HPV subtypes infection in the population.
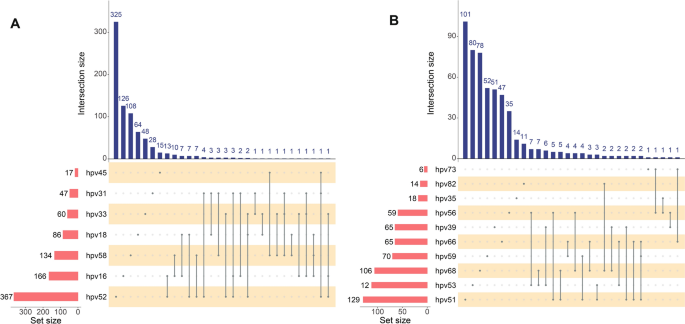
Furthermore, the distribution of nine-valent HPV vaccine-covered high-risk HPV subtypes and non-nine-valent HPV vaccine-covered high-risk HPV subtypes is shown in Fig. 2. Among them, the most common in nine-valent HPV vaccine-covered high-risk HPV subtypes were HPV 52 and 16, followed by 58, 18 and 33. Co-infection with HPV 16 and HPV 52, HPV 16 and HPV 58 were the most common type of multiple infection. As for non-nine-valent HPV vaccine-covered high-risk HPV subtypes, HPV51, 53, 68, 59 and 66 were the most common infections. Co-infection with HPV 53 and 56, HPV 53 and 68 were the most common multiple infection.
Correlation between HPV subtype infection and maternal outcomes
Next, we continued to analyze the relationship between HPV subtype infection and maternal pregnancy outcomes. Our findings indicated that HPV infection increases the risk of HDCP (OR = 1.40, (95%CI) (1.04–1.87)) and cesarean section (OR = 1.19, (95%CI) (1.05–1.35)). Further subgroup analysis showed that the incidence of both PPROM and cesarean section is significantly higher in the group II , suggesting that nine-valent HPV vaccine-covered HPV subtypes infection increases the risk of PPROM (OR = 1.29, (95%CI) (1.08–1.55)) and cesarean section (OR = 1.25, (95%CI) (1.06 to 1.49)). Besides, The results further indicated that pregnant women with co-infection with nine-valent HPV vaccine-covered HPV subtypes and non-nine-valent HPV vaccine-covered HPV subtypes had a cesarean section (OR = 1.59, (95%CI) (1.11–2.27)). Hypertensive disorders of pregnancy (HDCP) (OR = 2.73, (95%CI) (1.44 to 5.15)) had the highest risk. However, there was no statistical difference in the incidence of HPV infection and these complications, such as gestational diabetes (GDM), placental abruption and postpartum haemorrhage during pregnancy (Table 2).
Adjusted OR means adjusted for maternal age, Gravidity, Parity and Baby sex. *P < 0.05.
GDM, gestational diabetes; HDCP, hypertensive disorder complicating pregnancy; PPROM, preterm premature rupture of membranes; Control group means without HPV infection; group I means low risk HPV infection; group II means infection with nine-valent HPV vaccine covered high-risk HPV subtypes; group III means infection with non-nine-valent HPV vaccine covered high-risk HPV subtypes; group IV means co-infection with nine-valent HPV vaccine covered high-risk HPV subtypes and non-nine-valent HPV vaccine covered high-risk HPV subtypes.
Correlation between HPV subtype infection and neonatal outcomes
To further investigate whether HPV subtype infection affected pregnancy outcomes in newborns. The results of the multiple logistic regression analysis demonstrated that nine-valent HPV vaccine-covered high-risk HPV subtypes infection and co-infection HPV subtypes can significantly increase the risk of small for gestational age (SGA). Group IV(OR = 2.07, (95%CI) (1.21–3.54)) had a higher risk than the group III(OR = 1.33, (95%CI) (0.17–1.65)). In addition, we found that the risk of ICU admission in maternal with co-infection HPV subtypes significantly increased (OR = 1.58, (95%CI) (1.01–2.49) (Table 3).
Adjusted OR means adjusted for maternal age, Gravidity, Parity and Baby sex. *P < 0.05.
SGA,small for gestational age; LGA, large for gestational age; LBW, low birth weight infant; NICU, neonatal intensive care unit; Control group means without HPV infection; group I means low risk HPV infection; group II means infection with nine-valent HPV vaccine covered high-risk HPV subtypes; group III means infection with non-nine-valent HPV vaccine covered high-risk HPV subtypes; group IV means co-infection with nine-valent HPV vaccine covered high-risk HPV subtypes and non-nine-valent HPV vaccine covered high-risk HPV subtypes.