Mucormycosis, a fungal infection caused by Mucorales, has high mortality rates in people with weakened immune systems and those suffering from severe trauma like burns, blast injuries or victims of natural disasters. The disease caused serious infection among COVID-19 patients treated with high doses of corticosteroids with mortality rates close to 60 percent. In the United States, there are approximately 4,000 cases per year with a rate of 200,000 in Southeast Asia where the disease is endemic to India. While vaccines and immunotherapies are available for viruses and bacteria, effective antifungal immunotherapies for mucormycosis, specifically, are lacking.
Ashraf Ibrahim, Ph.D., an investigator at The Lundquist Institute for Biomedical Innovation at Harbor-UCLA Medical Center for more than 33 years, and Assistant Research Scientist, Yiyou Gu, Ph.D., at TLI for more than eight years, have been conducting research using monoclonal antibodies to address this gap.
Ibrahim’s research focuses on advancing the understanding of the pathogenic mechanisms and virulence factors of fungal and bacterial infections, and on translating this knowledge into novel immunotherapeutic strategies to combat infectious diseases.
Their paper, “A humanized antibody against mucormycosis targets angioinvasion and augments the host immune response,” was recently accepted and published in the Science Translational Medicine journal. In it, they discuss the use of monoclonal antibodies to target a key fungal cell surface protein, CotH, which enables the fungus to invade human cells and cause mucormycosis. Their findings will increase the efficiency of the current treatment options and thus will improve the outcome of treatment of lethal mucormycosis.
“Mucormycosis is a devastating disease that usually occurs in patients who suffer from weakened immune system such as patients with poorly controlled diabetes, cancer patients undergoing chemotherapy, and transplant patients,” said Ibrahim, adding that the disease has had a steady increase over the last four decades due to an increase in people with diabetes and cancer, as well as advancement in transplant procedures.
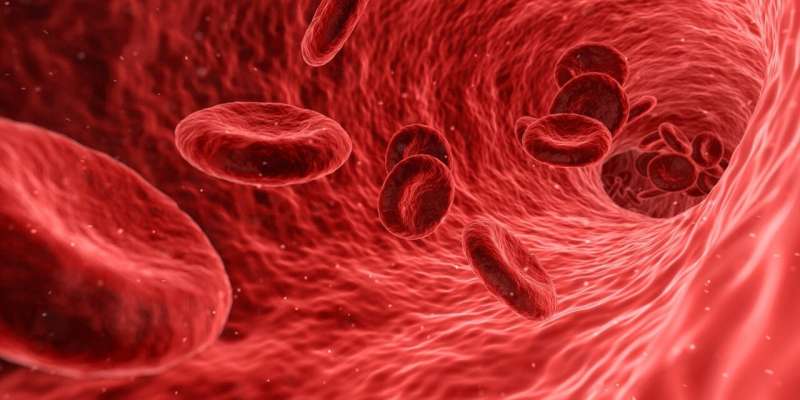
The infection is aggressive and considered a medical emergency that needs immediate attention, often with disfiguring surgery to remove infected tissues. The damage to blood vessels is concerning because it’s how antifungal drug therapy is delivered to the infection site. “Our humanized monoclonal antibody allows antifungal drug therapy to reach to infected tissues because it prevents fungal cells from damaging human cells and blood vessels,” Ibrahim said.
As a result, Ibrahim and Gu developed an antibody called VX-01, a humanized antibody that has proven more effective at binding to the fungus compared to the original antibody. Although both protect from infection, the humanized antibody reduces immunogenicity and enhances therapeutic effect when used in humans, a major translational step.
Early tests show that VX-01 is safe, with no harmful effects on healthy cells, suggesting that VX-01 could be a promising treatment to help fight mucormycosis in people with weakened immune systems.
The Lundquist Institute holds both U.S. and international patents for this humanized antibody and has granted Vitalex, a Lundquist spin-off company, the commercial rights to advance this therapeutic for Mucormycosis to patients.
More information:
Yiyou Gu et al, A humanized antibody against mucormycosis targets angioinvasion and augments the host immune response, Science Translational Medicine (2025). DOI: 10.1126/scitranslmed.ads7369
Provided by
The Lundquist Institute
Citation:
Antibody-based therapy is several steps closer to treat lethal mucormycosis (2025, March 22)
retrieved 22 March 2025
from https://medicalxpress.com/news/2025-03-antibody-based-therapy-closer-lethal.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.