Search results
Initially, 2,230 records were identified from the main databases. Following the removal of 294 duplicate records, 1,936 were screened. Of these, 1,767 records were excluded due to non-relevant participants, outcomes, or study design of interest. Subsequently, 169 articles were sought for full-text retrieval, all of which were successfully retrieved. During the eligibility assessment, 162 articles were excluded, primarily from conference abstracts, reviews, and studies lacking relevant information on syphilis in blood donors. Of the seven studies identified as eligible from the main databases, an additional four were found by searching 200 articles in Google Scholar. Furthermore, ten articles in Thai were identified from the TCI. A review of reference lists from the main databases and TCI yielded two more relevant articles. Twenty-three studies were included in the final review (Fig. 1).
Characteristics of included studies
Table 1 summarizes the characteristics of the 23 studies included in the review. The studies span several decades, with 26.1% published before 2000, 17.4% between 2000 and 2009, 34.8% between 2010 and 2019, and 21.7% from 2020 to 2024. Most of the studies (82.6%) utilized a retrospective descriptive design, while a smaller portion consisted of cross-sectional (13.0%) and retrospective case-control (4.4%) studies. Geographically, the research was distributed across various regions of Thailand, with Central and Northern Thailand each contributing 21.7% of the studies, followed by Lower Northern Thailand (17.4%), Northeastern Thailand (13.0%), and Southern, Western, and Eastern Thailand each representing 8.7%. Regarding diagnostic methods for syphilis, nearly half of the studies (47.8%) used nontreponemal serology, 26.1% used treponemal serology, 21.7% employed both, and 4.35% did not specify the diagnostic method used. Details of studies included in the systematic review and meta-analysis are shown in Table S2.
Risk of bias across included studies
In the cross-sectional studies27,28,29, all met the key criteria, including valid and reliable measurement of both exposure and outcomes (Table S3). However, some were limited regarding unclear inclusion criteria27 and a lack of attention to confounding factors27,29. All studies for prevalence studies10,11,12,13,14,15,30,31,32,33,34,35,36,37,38,39,40,41,42,43 met the key criteria, including appropriately sampled study participants and using valid methods for identifying the condition. However, some were limited regarding the unclear adequacy of the sample size15,33,36,40,42, insufficient detail on study subjects and settings11,37,41, and unclear use of appropriate statistical analysis13,31,33,36,37,41. None of the studies included in the systematic review were excluded based on the JBI checklist criteria.
Prevalence of syphilis among blood donors in Thailand
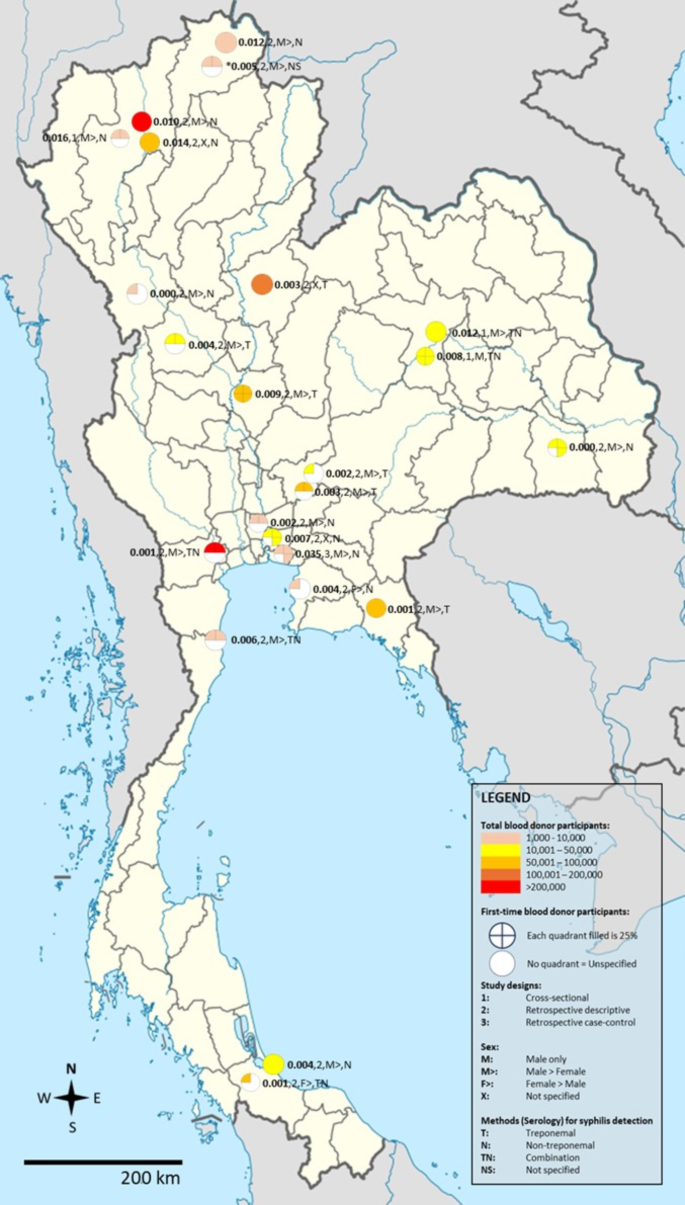
The pooled prevalence of syphilis among blood donors was estimated through a random-effects model based on data from 23 studies involving 1,142,910 blood donors. The meta-analysis results using random-effect models showed that the pooled prevalence of syphilis among blood donors in Thailand was 0.42% (95% CI [0.27%; 0.66%], I²: 99.3%, number of infections: 6,173, Fig. 2). The geographic distribution of the proportion of syphilis in Thailand is demonstrated in Fig. 3.
Permission is granted to copy, distribute and/or modify this document under the terms of the GNU Free Documentation License, Version 1.2 or any later version published by the Free Software Foundation.
Geographic distribution of the proportion of syphilis in Thailand. All studies had participants in the age range of 16 to 70 years. *All studies had 100% Thai nationality as participants except for Meepradit et al., 2022 in Mae Sai Hospital, Chiang Rai province (Thai: 4,873; 93.4%; Myanma/Burmese: 344; 6.6%). The template of the map was available at https://commons.m.wikimedia.org/wiki/File:Thailand_location_map.svg. This map template is licensed under the Creative Commons Attribution 3.0 Unported license.
The meta-regression analysis suggested that the high heterogeneity of the prevalence (I²: 99.3%) was due to several confounders, including publication years (P < 0.0001), study design (P = 0.0028), male percentage (P < 0.0001), and the proportion of first-time donors (P = 0.0189) (Supplementary Table S4). Subgroup analysis revealed that the pooled prevalence of syphilis among blood donors in Thailand was highest in studies published before 2000 (1.26%) and decreased during 2000–2009 (0.94%), 2010–2019 (0.27%), and 2020–2024 (0.20%) (Supplementary Table S5). The bubble plot revealed a significant trend of decreasing prevalence of syphilis among blood donors in Thailand from 1995 to 2024 (Supplementary Fig. 1). A difference in prevalence was also observed, with three cross-sectional studies showing a higher prevalence than retrospective descriptive studies (1.13% vs. 0.32%). The subgroup analysis further revealed that Northern Thailand had the highest pooled prevalence compared to other regions (1.08%), although the number of included studies in each subgroup varied. Using serological (nontreponemal) techniques for the detection of syphilis resulted in the highest pooled prevalence (0.51%) compared to other methods (Supplementary Table S5).
Association between gender and risk of syphilis
The association between gender and syphilis in blood donors was estimated using the data from 11 studies that reported the available data for pooling the OR12,14,15,28,30,32,34,35,36,39,42. The meta-analysis results using random-effect models demonstrated that male blood donors were associated with increased risk for syphilis (P < 0.0001; pooled OR: 1.76; 95% CI [1.53; 2.03]; I²: 34.2%, number of participants: 651,019; Fig. 4). Non-significant heterogeneity was observed in the meta-analysis (P = 0.13), with a low degree of heterogeneity. Therefore, meta-regression and subgroup analyses were not conducted.
Association between frequency of donations and risk of syphilis
The association between the frequency of donations and the risk of syphilis in blood donors was estimated using the data from nine studies that reported the available data for pooling the OR12,14,28,30,31,32,33,34,36. The meta-analysis results using random-effects models demonstrated that first-time donations were associated with an increased risk of syphilis (P = 0.023; pooled OR: 2.02; 95% CI [1.10; 3.70]; I²: 94.0%, number of participants: 215,245; Fig. 5). The high heterogeneity observed in the meta-analysis may have been caused by the regions of Thailand or methods for syphilis detection, as suggested by the subgroup analysis (Supplementary Table S6).
Association between age of blood donors and risk of syphilis
The meta-analysis compared the age of blood donors, and the risk of syphilis revealed that participants aged 21–30 years, 31–40 years, and 41–60 years exhibited significantly increased risks of syphilis compared to those aged 17–20 years (OR: 1.63; 3.92; 6.91). Similarly, participants aged 31–40 years and 41–60 years showed significantly higher syphilis risk relative to the 21–30 age group (OR: 2.50; 4.31). Interestingly, participants aged 41–60 years displayed a significantly increased risk of syphilis in comparison to those aged 31–40 years (OR: 1.83, Supplementary Table S7; Supplementary File 1).
Sensitivity analysis
For the meta-analysis of the pooled prevalence, the meta-analysis results using fixed-effects models demonstrated that the pooled prevalence of syphilis among blood donors in Thailand was 0.54% (95% CI [0.53%; 0.55%], I²: 99.3%, Fig. 2). For the association between gender and risk for syphilis, the meta-analysis results using fixed-effects models demonstrated that male blood donors were associated with increased risk for syphilis (P < 0.0001; pooled OR: 1.87; 95% CI [1.73; 2.03], Fig. 4). Influential analysis using the random-effects model revealed that after each study was removed and the meta-analysis rerun, the results remained unchanged (P < 0.0001, Supplementary File 2). For the association between frequency of blood donations and risk for syphilis, the meta-analysis results using fixed-effects models demonstrated similar findings in which first-time donations were associated with increased risk for syphilis (P < 0.0001; pooled OR: 2.04; 95% CI [1.76; 2.36], Fig. 5). Influential analysis using the random-effects model revealed that after each study was removed and the meta-analysis rerun, the meta-analysis results were changed by some studies30,31 (P < 0.05, Supplementary File 3). The removal of these studies led to a slight increase in the pooled effect size, suggesting that the lower male percentage in these studies may have contributed to a lower overall risk estimate in the original analysis, as demonstrated by Burananayok et al.30.
Publication bias
In the meta-analysis of the pooled prevalence, the funnel plot showed an asymmetrical distribution of prevalence estimates among the included studies relative to the central line (Supplementary Fig. 2). Additionally, Egger’s test revealed significant funnel plot asymmetry (P = 0.03), indicating the presence of publication bias in the meta-analysis of the pooled prevalence. For the association between gender and the risk of syphilis, the funnel plot showed an asymmetrical distribution of ORs among the included studies relative to the central line (Supplementary Fig. 3). Additionally, Egger’s test revealed a funnel plot symmetry (P = 0.32), indicating the absence of publication bias in the meta-analysis of the OR. For the associations between the frequency of blood donations and the risk of syphilis, as well as between the age of participants and the risk of syphilis, funnel plots were not generated because the number of included studies was less than 10.










