Researchers from Saint Louis University recently conducted a study revealing that only 1 out of 8 heart failure patients in the US receive palliative care consultation within five years after being diagnosed.
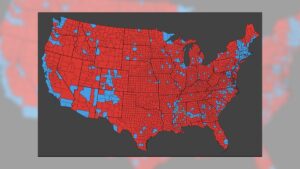
Recent findings published by the Journal of the American Heart Association highlight a remarkable lack of palliative care utilization among adults living with heart failure in America compared to cancer patients battling similar fatal conditions. Furthermore, significant racial and geographic disparities exist; Black people were 15% less likely than their white counterparts to receive palliative care services.
Given Black people’s greater risk and mortality rates for cardiovascular disease, this disparity is especially concerning. Over the last decade, both the American Heart Association (AHA) and European Society of Cardiology have recommended including palliative care services as part of managing heart failure.
Anecdotal reports show that most heart failure patients do not receive palliative care, with those receiving it typically doing so only within their last two or three weeks of life.
Zidong Zhang, PhD. is an assistant research scientist in SLU’s AHEAD Institute School of Medicine and co-senior/corresponding author on this paper.
Zhang, an accomplished health service researcher specializing in palliative and patient-centric care for cardiovascular disease and cancer patients, has presented his studies at national conferences. Furthermore, they were published in peer-reviewed journals.
“To our knowledge, this study marks the first attempt to investigate uptake of palliative care consultation after heart failure diagnosis in the general U.S. population compared with prior research which focused on Medicare beneficiaries or veterans exclusively,” explained Professor Leech.
Zhang and his co-authors conducted this retrospective analysis from 2011-2018 by using data from a national all-payer database, comprising nearly 170,000 patients aged 18-80 from all country regions who suffered advanced heart failure or received advanced treatments such as left ventricular assist devices or cardioversion. Furthermore, this research demonstrated the heterogeneous relationship between palliative care options for acute heart failure patients and any further worsening.
Zhang and his co-authors observed that patients not suffering from cardiogenic shock – an emergency condition where your heart suddenly cannot pump enough blood to meet your body’s demands – yet receiving inotropic therapy, medications that tell heart muscle cells how powerfully to contract or beat, were less likely to seek palliative care consultations; in comparison with advanced therapies intended to treat cardiogenic shock cases which nearly tripled that likelihood attributed by Zhang et al. as being caused by their intended purpose as well as clinical inertance in handling complex cases managed.
Zhang noted the AHA guidelines emphasize early integration of palliative care consultation for all heart failure patients being evaluated for advanced therapies; however, study data show there may be discrepancies between this recommendation and real world practice; Zhang suggested systemic reform would enable early integration and timely consultation for palliative care services.
“These may include eliminating barriers in the payment system for concurrent care, helping physicians determine when it is time to initiate palliative care conversations with patients and increasing community-based palliative care services and streamlining referral and transition of cardiac palliative care to inpatient services and finally outpatients in health systems,” according to Pike.
Additional contributors of the report were: Divya S. Subramaniam, Ph.D. of Saint Louis University School of Medicine’s Department of Health and Clinical Outcomes/AHEAD Institute; Steven W. Howard, Ph.D. from University of Alabama at Birmingham; Kenton Johnston Ph.D. from Department of Internal Medicine Washington University School of Medicine; William H Frick M.D of Department of Internal Medicine Saint Louis University School of Medicine; Kimberly Enard Ph.D of College for Public Health/Social Justice Saint Louis University as well as Leslie Hinyard’s Phd thesis research work at Saint Louis University’s Department/AHEAD Institute/AHEAD Institute; Steven W Howard is from University Alabama at Birmingham while Kenton Johnston Ph.D. from Department of Internal Medicine Washington University School of Medicine in Saint Louis University’s Department of Internal Medicine at Washington University School of Medicine while William Frick M.D. of Saint Louis University’s Internal Medicine Department as well as Leslie Hinyard Phd of Department/Health and Clinical Outcomes and Ahead Institute/Saint Louis University’s Saint Louis School of Medicine’s department/AHEAD Institute/Saint Louis University School of Medicine in Saint Louis School.
Journal Reference: Zhang, Z. and coauthors (2024). Exploration of Palliative Care among Adults With Newly Diagnosed Heart Failure in an US National Insured Patient Sample. Journal of the American Heart Association; DOI 10.1161/jaha.124.035459.
![[original_title]](https://rawnews.com/wp-content/uploads/2024/11/patient_support_pallative_care_-_Photographee.eu_ab1fca8683ee4d9c86906391b326aa46-620x480.jpg)